Denied insurance claims can feel like a dead end—frustrating, confusing, and financially overwhelming. But what many people don’t realize is that a thorough, strategic approach to medical record reviews – claim appeal can make all the difference. At Gables Medical Review, we’ve seen firsthand how a detailed record review can uncover what’s missing, clarify medical necessity, and ultimately overturn denied claims. This blog walks through how we do it—and why it works.
Understanding the Importance of Medical Record Reviews
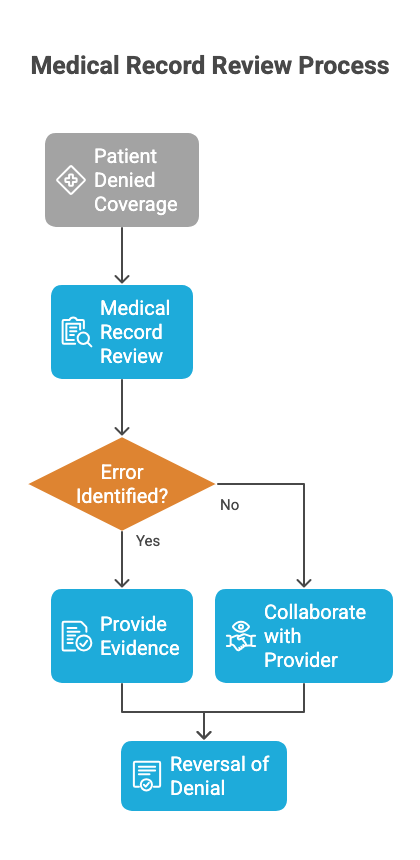
When a claim is denied, it often boils down to insufficient evidence or documentation that doesn’t clearly support the treatment or procedure. That’s where medical record reviews come in. We comb through every note, test result, and report to build a case that presents the patient’s condition in full context—helping support a solid claim appeal.
Through this process, we identify the gaps, correct any inconsistencies, and provide insurance companies with a comprehensive, accurate picture of why the claim should be paid. We’ve built our entire approach at Gables Medical Review around using these reviews to unlock reversals and reimbursement success.
The Role of Gables Medical Review
At Gables Medical Review, we specialize in conducting thorough and objective medical record reviews. Our team of experts works diligently to ensure that every aspect of the patient’s medical history is considered. This includes reviewing physician notes, diagnostic results, treatment plans, and any other pertinent documentation. By offering a detailed and unbiased evaluation, we provide the necessary insights to support a successful claim appeal.
Common Reasons for Claim Denials
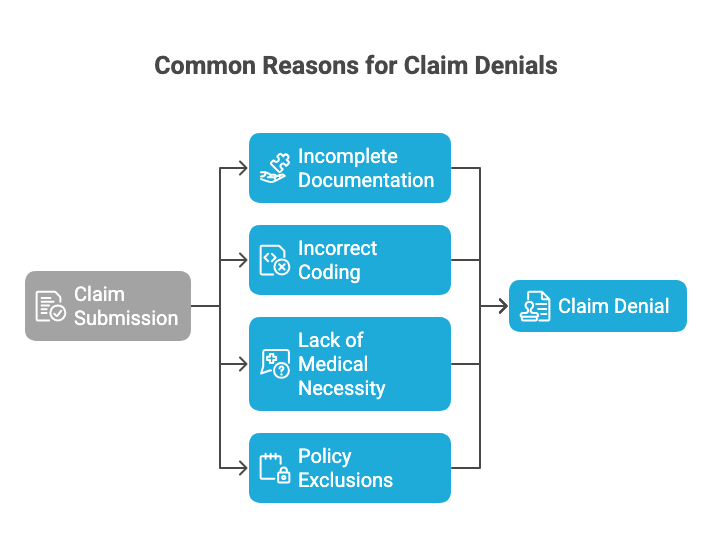
To effectively overturn a denied claim, it’s essential to understand the common reasons why claims are denied in the first place. Some of the most frequent causes include:
Common Reasons for Claim Denials
- Incomplete Documentation: Missing or incomplete medical records can lead to a lack of evidence for the necessity of a procedure or treatment.
- Incorrect Coding: Errors in medical coding can result in claims being categorized incorrectly, leading to denials.
- Lack of Medical Necessity: Insurance companies often deny claims if they believe a treatment is not medically necessary.
- Policy Exclusions: Some treatments may be excluded from coverage based on the insurance policy terms.
Each of these issues can be addressed through a comprehensive medical record review. By identifying and correcting these problems, we can present a stronger case for the claim appeal.
Strategies for Successful Record Reviews
Conducting a successful medical record review requires a strategic approach. Here are some key strategies that we employ at Gables Medical Review:
- Thoroughness: We meticulously examine every piece of documentation to ensure no detail is overlooked.
- Collaboration: We work closely with healthcare providers to gather additional information or clarifications when necessary.
- Expert Analysis: Our team includes medical professionals who understand the nuances of medical terminology and procedures.
- Clear Communication: We provide clear and concise reports that outline our findings and support the appeal process.
By following these strategies, we can significantly increase the likelihood of overturning denied claims.
The Impact of Successful Claim Appeals
When a denied claim is successfully appealed, the impact can be profound. Patients gain access to the medical treatments they need without the burden of unexpected costs. Healthcare providers receive the compensation they are due for the services rendered. Moreover, a successful appeal can set a precedent for future claims, potentially simplifying the process for similar cases.
At Gables Medical Review, we take pride in our track record of helping clients achieve favorable outcomes. Our commitment to excellence and attention to detail have made us a trusted partner in the claim appeal process.
Case Studies: Real-Life Success Stories
To illustrate the effectiveness of medical record reviews, let’s explore a few real-life success stories:
- Case Study 1: A patient was denied coverage for a necessary surgical procedure due to a coding error. Our team identified the mistake during the record review and provided evidence that led to the reversal of the denial.
- Case Study 2: In another instance, a claim was denied because the insurance company deemed the treatment experimental. Our review uncovered documentation proving the treatment’s established efficacy, resulting in a successful appeal.
- Case Study 3: A routine claim for physical therapy was denied due to missing documentation. We collaborated with the healthcare provider to obtain the necessary records, leading to the approval of the claim.
These examples demonstrate the tangible benefits of a thorough and well-executed medical record review.
We believe that behind every denied claim is a story waiting to be told—and the way to tell it is through a clear, accurate, and strategic record review. Whether it’s correcting documentation, clarifying medical necessity, or reinforcing provider credibility, medical record reviews – claim appeal is one of the most powerful tools available to change the outcome.
If you’re dealing with a denial or working on a tough appeal, let us help. At Gables Medical Review, we’re committed to supporting providers and patients with the insights needed to fight back. Get in touch with us today and see how we can help overturn denied claims with precision and expertise.