Navigating healthcare insurance can feel like an endless maze of paperwork, codes, and deadlines—especially when a claim gets denied. Patients and providers alike often ask, “How do I appeal an insurance claim denial?” That’s where expert guidance becomes essential. At Gables Medical Review, we specialize in Insurance Claim Review and Denial Appeals, helping clients take control of their claims, resolve denials efficiently, and achieve fair, accurate outcomes. Our mission is simple: to simplify the process, maximize approvals, and empower every step of your healthcare journey.
Understanding the Insurance Claims Process
The insurance claims process can be overwhelming without the right support. Each step—from verifying codes to interpreting policy terms—requires careful attention. Missing a single detail can result in claim rejections or costly delays.
Why Claims Get Denied
Insurance claim denials can occur for a myriad of reasons. Some common causes include:
- Incorrect or incomplete information
- Non-covered services
- Lack of pre-authorization
- Missed deadlines for submission
- Policy exclusions or limitations
Understanding these causes is crucial to prevent future denials. But when a claim is rejected, knowing how to appeal an insurance claim denial effectively can make all the difference.
How Gables Medical Review Can Help
At Gables Medical Review, our focus is to take the complexity out of Insurance Claim Review and Denial Appeals. We use a proven, systematic approach to ensure your claims are accurate, timely, and well-supported.
Comprehensive Claim Review
Our comprehensive claim review process involves a detailed examination of your insurance claims to identify any potential issues that may lead to denials. We check for errors, validate billing codes, and ensure compliance with policy terms. By catching these issues early, we help prevent denials and expedite the reimbursement process.
Expert Denial Appeals
When a claim is denied, we step in to help you navigate the appeals process confidently. Our experts know how to appeal an insurance claim denial—from understanding denial codes to assembling compelling evidence and supporting documentation. We craft persuasive appeals that stand up to insurer scrutiny and fight for the reimbursement you rightfully deserve.
Our Proven Process
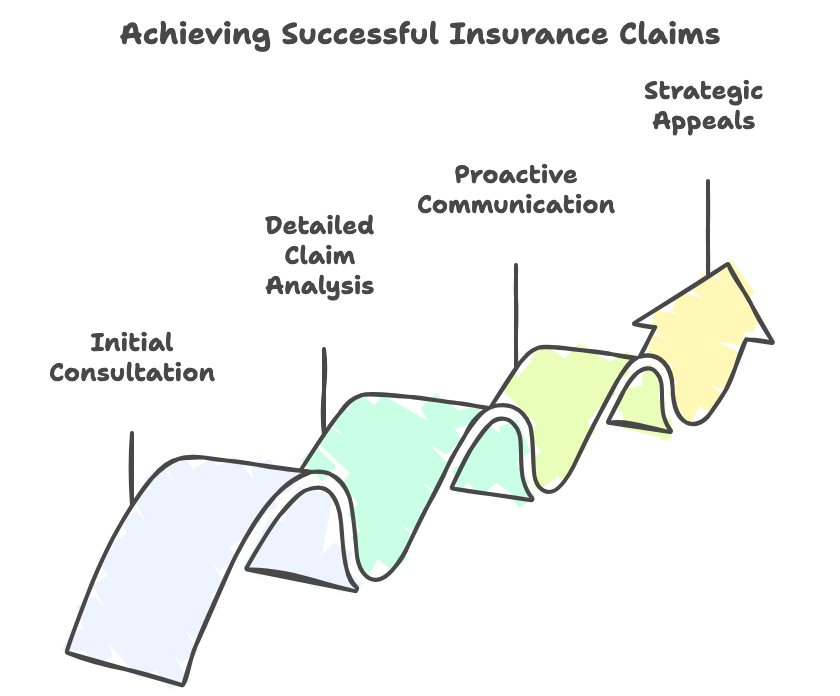
At Gables Medical Review, we follow a structured process to streamline your insurance claims and maximize your success rate. Our approach includes:
1. Initial Consultation
We begin with an initial consultation to understand your specific needs and challenges. This allows us to tailor our services to your unique situation and develop a strategy that aligns with your goals.
2. Detailed Claim Analysis
Our team conducts a thorough analysis of your claims, checking for errors, discrepancies, and compliance with policy terms. We leverage our expertise to ensure that every claim is accurate and complete before submission.
3. Proactive Communication
Communication is key in the claims process. We maintain proactive communication with insurers, healthcare providers, and clients to ensure that all parties are informed and aligned. This minimizes delays and enhances the likelihood of successful claims.
4. Strategic Appeals
In the event of a denial, we act swiftly to prepare a strategic appeal. Our team gathers supporting documentation, constructs compelling arguments, and submits the appeal within the required timeframe. We are relentless in our pursuit of fair and accurate claim resolutions.
Empowering Your Healthcare Journey
Working with Gables Medical Review means gaining a dedicated partner who simplifies the insurance process and advocates for your success. We handle the details so you can focus on your health and peace of mind.
Benefits of Our Services
Our services offer numerous benefits, including:
- Time Savings: We handle the complex and time-consuming aspects of claims management, freeing you to focus on your health.
- Financial Security: By maximizing claim approvals, we help secure the financial resources needed for your healthcare.
- Peace of Mind: Knowing that a team of experts is managing your claims provides peace of mind and reduces stress.
Why Choose Gables Medical Review?
Choosing us means choosing precision, transparency, and commitment. Our personalized service ensures every client feels supported and informed. Whether you’re a patient or provider, our team approaches your claim as if it were our own—because your success is our priority.
Client Testimonials
Our success is reflected in the satisfaction of our clients. Here are some testimonials from those who have benefited from our services:
- “Gables Medical Review turned my claim denial into an approval. Their expertise and dedication are unmatched.” – John D.
- “Thanks to Gables Medical Review, I no longer stress over insurance claims. They handle everything with professionalism and care.” – Sarah P.
- “The team at Gables Medical Review is knowledgeable, responsive, and truly cares about their clients’ success.” – Emily R.
If you’ve been struggling with complex claims or unanswered denials, it’s time to take control. Contact Gables Medical Review to schedule a consultation. We’ll review your case, guide you through the process, and help you achieve faster, more successful results.
At Gables Medical Review, we don’t just process claims—we protect your rights, your time, and your peace of mind. Let us help you navigate the world of Insurance Claim Review and Denial Appeals with confidence and clarity.